Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Every four minutes, a woman in India is diagnosed with breast cancer. That’s not just a number—it’s a powerful reminder of a growing crisis. What was once the fourth most common cancer among Indian women in the 1990s has now become the most widespread, turning into a major public health concern across the country.
According to a recent study published in Nature Journal, the number of Indian women undergoing breast cancer treatment is expected to increase by 50,000 annually over the next decade. The financial toll is just as alarming, with the average annual cost estimated at $19.55 billion. Factors like genetics, obesity, unhealthy lifestyles, poor diets, smoking, and alcohol use are all playing a part in this sudden surge. But in India, the situation is even more complex. Women here are being diagnosed at younger ages compared to those in Western countries, and the disease often behaves more aggressively in younger patients—making treatment more difficult and outcomes more severe.
“The biological features of breast cancer in younger women are more aggressive and increase the chances of relapse and spread,” the report highlights, “which leads to poorer outcomes than in older women.”
A government report presented in the Lok Sabha in 2024 provided insight into how serious the situation has become. Between 2019 and 2023, breast cancer cases rose from 200,218 to 221,579, and deaths increased from 74,481 to 82,429. While more women are being diagnosed early, the growing death toll reveals deep-rooted problems in early detection, treatment access, and healthcare infrastructure.
Figure 1 : Estimated number of Breast Cancer incidence and mortality rate from (2019-2023) in India among female
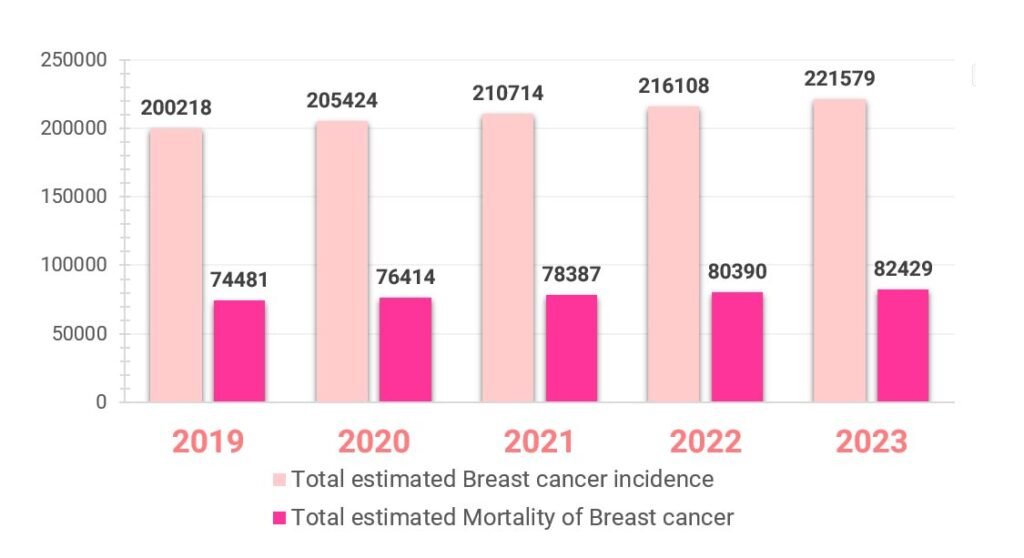
Source: Sansad Document
Rising numbers are just one part of the story. There are multiple challenges adding to the burden. One major issue is the late diagnosis of the disease. In India, around 60% of breast cancer patients are diagnosed at Stage III or IV, where survival chances are significantly lower. While Stage I patients have a survival rate of around 93.3%, it drops drastically to 24.5% for those in Stage IV.
One of the root causes is lack of awareness. Many women in India, especially in rural and economically weaker areas, aren’t informed about breast cancer symptoms or the importance of regular check-ups. Cultural taboos, fear, and stigma around the disease often stop women from seeking help.
The NFHS data from 2019-2021 reveals a shocking truth—only 0.9% of women aged 30 to 49 have ever undergone a breast cancer screening. This is compounded by poverty, low education levels, poor healthcare access, and the geographical inaccessibility of medical facilities.
“Breast-health-related stigmas worsen the situation, making women hesitate to speak up or get medical advice,” a health official said during a campaign.
Efforts like the “Pink Month” campaign aim to spread awareness and encourage women to get screened early. However, the ground reality remains grim.
India’s healthcare infrastructure still struggles to meet the demands of early breast cancer detection and treatment. There’s a shortage of advanced screening tools like mammography machines, especially outside metropolitan areas. Even where machines are available, issues such as high breast density in Indian women can reduce mammography accuracy, sometimes leading to false positives or overdiagnosis.
Another major challenge is the cost of treatment. Managing breast cancer in India can cost anywhere between ₹1 lakh to ₹10 lakh, depending on the type of care and duration of treatment. For many families, especially those from low-income backgrounds, this becomes a massive financial burden. Limited insurance coverage and out-of-pocket expenses often force patients to abandon treatment halfway through.

Nearly 40% of Indian hospitals still lack access to modern cancer care technology. Only a few centers across the country offer combined treatments like surgery, chemotherapy, and radiotherapy under one roof. Moreover, 95% of specialized cancer facilities are located in cities, making it nearly impossible for rural women to receive proper care. With only 2,000 oncologists available for over 10 million patients, the healthcare system is clearly overstretched.
Even newer, more advanced treatments like immunotherapy and targeted therapy are out of reach for most patients due to their high cost.
Beyond the physical illness, breast cancer carries a heavy emotional and psychological impact. A diagnosis often brings shock, fear, anger, anxiety, and deep sadness. Patients not only face a life-threatening disease but also worry about their families, jobs, and personal lives. The emotional weight can sometimes be just as devastating as the illness itself.

Despite these challenges, there are signs of progress and hope. One major area for improvement is public awareness. Campaigns led by both government and private organizations can play a major role in breaking cultural stigmas and educating women about early signs and prevention.
Educational institutions and workplaces can also contribute by hosting awareness drives and regular screenings. Including breast health as part of school and college curriculums can ensure that young women are informed early.

Healthcare workers, especially in rural areas, need to be trained to detect symptoms early. A powerful initiative in this space is the partnership between the University of East Anglia (UK) and India’s International School of Oncoplasty (ISOS) under the Prashanti Cancer Care Mission (PCCM). Their structured fellowship program is building capacity among Indian doctors by focusing on oncoplastics—a surgical approach that combines cancer removal with cosmetic breast preservation.
Technology is also stepping in. Tools like regenerative AI are now helping doctors identify cancer earlier and more accurately by analyzing mammograms, MRIs, and ultrasound scans. AI systems such as “MammoAssist” are improving diagnostic efficiency and easing the burden on medical professionals.

“MammoAssist has shown promising results in improving diagnostic accuracy through better mammogram analysis,” said one of the developers of the system.
Another success story is the Breast Health Initiative (BHI), which aims to train ASHAs (Accredited Social Health Activists), nurses, and midwives to conduct awareness and screening programs across India. These women, who are already embedded in their communities, are uniquely positioned to build trust and encourage others to participate in early detection programs.
India’s growing breast cancer burden calls for a comprehensive and urgent response. While the problems are complex and numerous, the opportunities for change are equally powerful. With stronger policies, better infrastructure, more awareness, and early detection programs, India can transform the way breast cancer is prevented and treated.
Regardless of a woman’s background, with the right support systems in place—both medical and emotional—breast cancer can become a manageable and survivable disease. It’s time for India to invest wisely, plan holistically, and bring communities together to win this fight.
How do you believe India can close the gap between breast cancer awareness and actual treatment access? Have you or someone you know experienced the challenges discussed here?
Share your thoughts—what’s your point of view on this growing health crisis?